Hydrocephalus is a pathological expansion of the spaces in the brain that are filled with cerebrospinal fluid (CSF). These so-called cerebral ventricles inflate when a CSF congestion occurs. Hydrocephalus can have numerous causes, be congenital or acquired. The aim of hydrocephalus treatment is always to restore the normal cerebrospinal fluid flow or to create an alternative outflow. At Inselspital, we have many years of expertise in the surgical treatment of hydrocephalus.
How common is hydrocephalus and what are the risk groups?
In childhood
In childhood, hydrocephalus mainly occurs due to congenital malformations. These are for example Chiari malformations, meningomyeloceles (congenital spinal cord malformations) or aqueduct stenoses. Somewhat less common are secondary hydrocephalus following meningitis, postnatal cerebral hemorrhage, or neurosurgical procedures.
In adults
In adulthood, the secondary forms of hydrocephalus come to the fore, which are due to blockages or drainage disorders. These occur after hemorrhages, infections, tumors, neurosurgical procedures, etc.
In geriatric patients
Normal pressure hydrocephalus (also known as age-related brain pressure), on the other hand, typically occurs in geriatric patients and is almost never seen in children and young adults.
What are the possible causes of hydrocephalus?
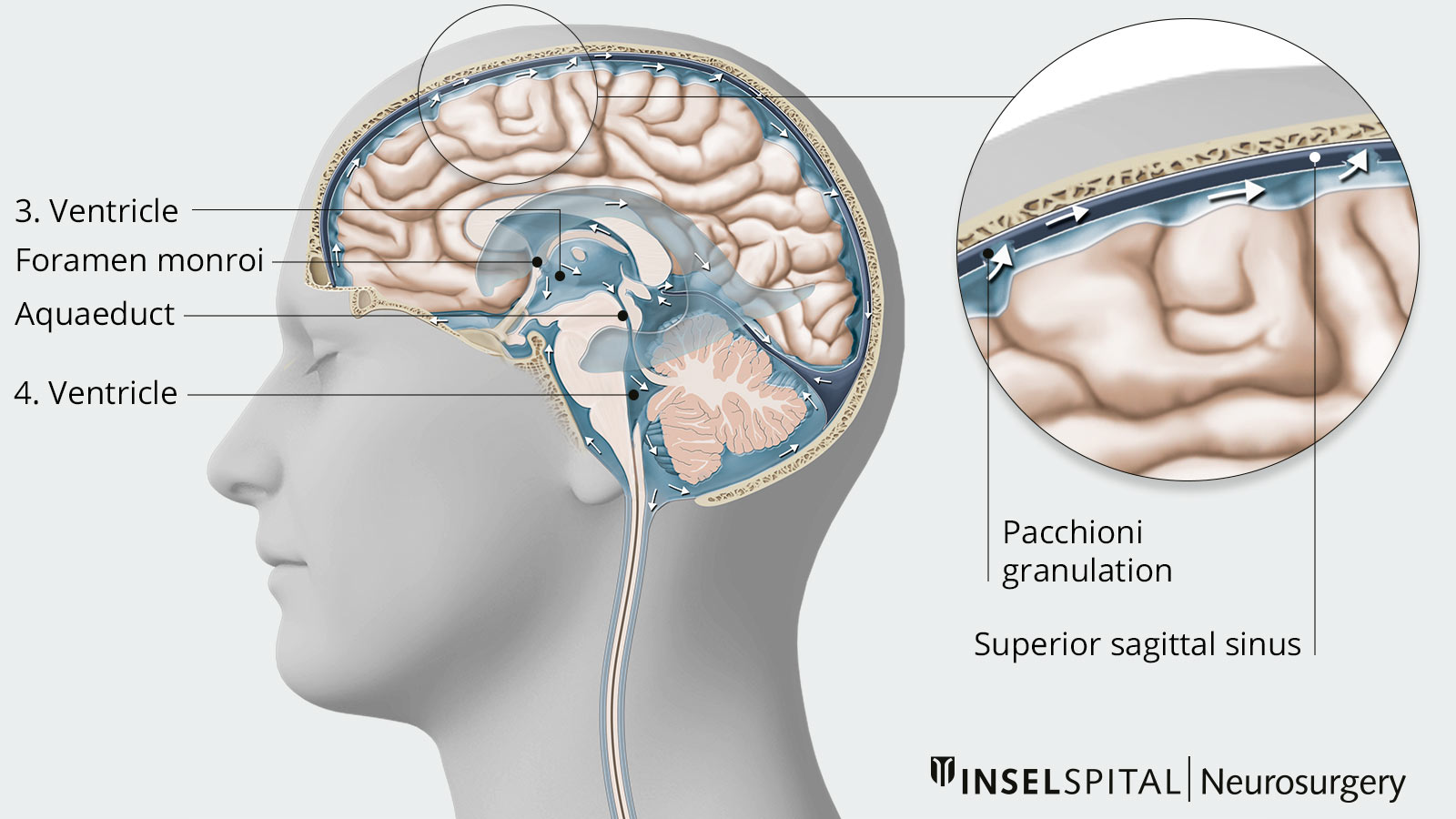
In order to understand the causes of hydrocephalus, one must briefly consider the ventricular system of the brain. It is composed of four brain chambers, the so-called ventricles, which are filled with cerebrospinal fluid (CSF) and lined with a thin layer of cells, the ependyma.
We differentiate between:
- 1st and 2nd ventricles (the paired lateral ventricles) each with connection via the foramen interventriculare (foramen Monroi) with the
- 3rd ventricle, which in turn is connected by the approx. 1 mm narrow aqueductus mesencephali with the
- 4th ventricle, which is connected to the external CSF spaces.
The cerebrospinal fluid is formed in the choroid plexus, which is located in all four brain ventricles, and after circulation through the ventricles it passes through openings into the external cerebrospinal fluid space outside the brain. Resorption into the bloodstream takes place here. In other words, it is a circulatory system in which production and outflow must be balanced in order for the intracranial pressure to remain constant.
The total CSF space holds approximately 150 ml of CSF (20% in the ventricles and 80% in the subarachnoid space). This amount is completely exchanged about three times a day, producing an estimated 450–500 ml of CSF per day. Increased production or outflow disturbances of the cerebrospinal fluid can cause hydrocephalus, which then leads to an increase in intracranial pressure.
In addition to the numerous causes, the symptoms and course of the disease often present differently, which is why hydrocephalus can be divided into the following subtypes:
- Hydrocephalus malresorptivus
This form of hydrocephalus is caused by impaired resorption of CSF in the Pacchioni granulations of the subarachnoid space. Reasons for this may be subarachnoid or ventricular hemorrhage, meningitis, meningoencephalitis, or meningeosis carcinomatosa (metastasis to the meninges). - Hydrocephalus occlusus or occlusive hydrocephalus
This form of hydrocephalus is caused by a mechanical blockage of the cerebrospinal fluid outflow in the area of the draining cerebrospinal fluid ducts. Tumors of any kind as well as cysts and aqueduct stenoses are among the most frequent causes. - Hydrocephalus e vacuo
This involves compensatory increased cerebrospinal fluid production with enlargement of the cerebrospinal fluid spaces following the destruction of healthy brain tissue and a decrease in the volume of the brain. This form does not lead to increased intracranial pressure. Causes of hydrocephalus e vacuo are, for example, dementia or neurodegenerative diseases such as Parkinson's disease, Alzheimer's disease, etc. - Hydrocephalus communicans or normal pressure hydrocephalus
Hydrocephalus communicans or normal pressure hydrocephalus is a distinct condition with reversal of CSF flow dynamics without flow obstruction and with little or no increase in pressure.
What are the symptoms of hydrocephalus?
Symptoms and complaints of hydrocephalus can be manifold. Basically, a distinction must be made between acute and chronic hydrocephalus.
Acute hydrocephalus
In this case, the pressure in the ventricular system increases within a very short time. As a result, patients suffer from classic intracranial pressure symptoms ranging from severe headaches, nausea and vomiting to clouding of consciousness and coma. Epileptic seizures may also occur.
Chronic hydrocephalus
The symptoms gradually increase over months or years in adults or older children. Typical symptoms include headaches, nausea and vomiting, blurred vision, gait disturbances, cognitive impairment and urinary incontinence.
Normal pressure hydrocephalus
In normal pressure hydrocephalus, there are usually no symptoms due to increased intracranial pressure. Typical for this clinical picture is a triad of 3 symptoms. The so-called Hakim triad includes gait disturbances, dementia and urinary incontinence.
How is hydrocephalus diagnosed?
The best examination method for imaging the ventricular system is computed tomography (CT). For specific questions and for detailed imaging of malformations, cysts or tumors that can lead to hydrocephalus, magnetic resonance imaging (MRI) is usually performed.
In the case of acute decompensation, when the body can no longer compensate for the cerebral hypertension, emergency imaging is always performed by means of a CT scan of the skull in order to be able to initiate therapy promptly.
A lumbar puncture can be used to measure the pressure in the CSF system. In occlusive hydrocephalus, lumbar puncture is contraindicated due to possible tonsillar entrapment.
How is hydrocephalus treated?
The goal of hydrocephalus treatment is to restore normal CSF flow or, if this is not possible, to create an alternative outflow.
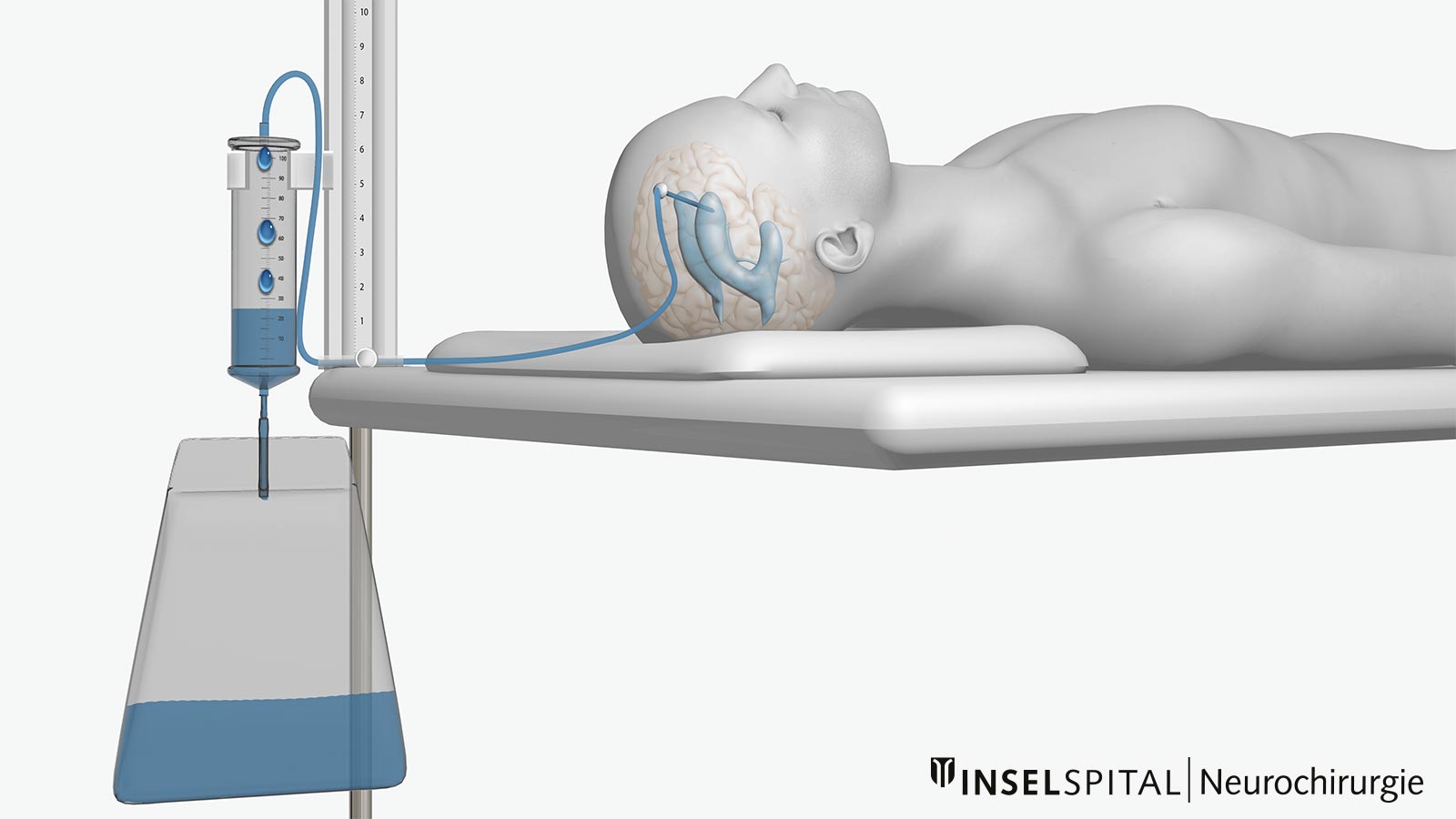
Relief by external ventricular drainage in emergency situations
Acute hydrocephalus with increased intracranial pressure (for example, due to a cerebral hemorrhage) can be relieved quickly and easily in an emergency situation by external ventricular drainage. In this procedure, a catheter is advanced into the ventricular system through a small burr hole in the skull (usually frontal on the right side, sometimes on both sides). This drainage allows the excess cerebrospinal fluid to flow into the connected system and the acute danger is averted. Modern ventricular catheters also allow continuous measurement of intracranial pressure.
In emergency situations, there are systems that allow safe and easy insertion of a ventricular drain directly at the patient's bedside, so that pressure relief can be achieved within minutes. However, external ventricular drainage is only appropriate as a temporary drain.
Microsurgical resection and third ventriculocisternostomy
In occlusive hydrocephalus, normal CSF flow may be restored by surgical removal of the obstruction to outflow. This may be, for example, microsurgical resection of a colloid cyst or resection of a tumor in the ventricular system. In cases where this is not possible or is very risky, the creation of an alternative outflow pathway may be considered. This is typically the case in aqueductal stenosis, where a minimally invasive endoscopic opening of the floor of the 3rd ventricle (third ventriculocisternostomy) is used to create an outflow into the prepontine cisterns. This procedure is also used for obstruction of the entrance to the aqueduct in the posterior part of the 3rd ventricle caused by tumors or cysts and has the advantage that an unclear process can be biopsied under endoscopic view during the procedure.
Ventriculoperitoneal shunt (VP shunt)
In the case of hydrocephalus communicans, drainage of the accumulated CSF in the ventricular system can be achieved via a ventriculoperitoneal shunt (VP shunt). This is a surgically created connection between the ventricular system and the abdominal cavity.
During surgery, a ventricular catheter is inserted through the cranial roof and into the ventricular system. The ventricular catheter can be placed precisely in the ventricular system using natural landmarks on the head and under sonographic view with an ultrasound device. A subcutaneous reservoir, which later allows puncture of the system (e.g., for pressure measurement or CSF examination), is then used to guide the catheter under the scalp to behind the ear, where it is connected to a valve system that is also implanted under the scalp. This valve later regulates intracranial pressure and CSF outflow volume and can be adjusted magnetically from the outside. From the valve, a long catheter runs subcutaneously from the neck across the chest to the abdomen. From here, the catheter is guided into the abdominal cavity, where the CSF is reabsorbed and fed into the bloodstream.
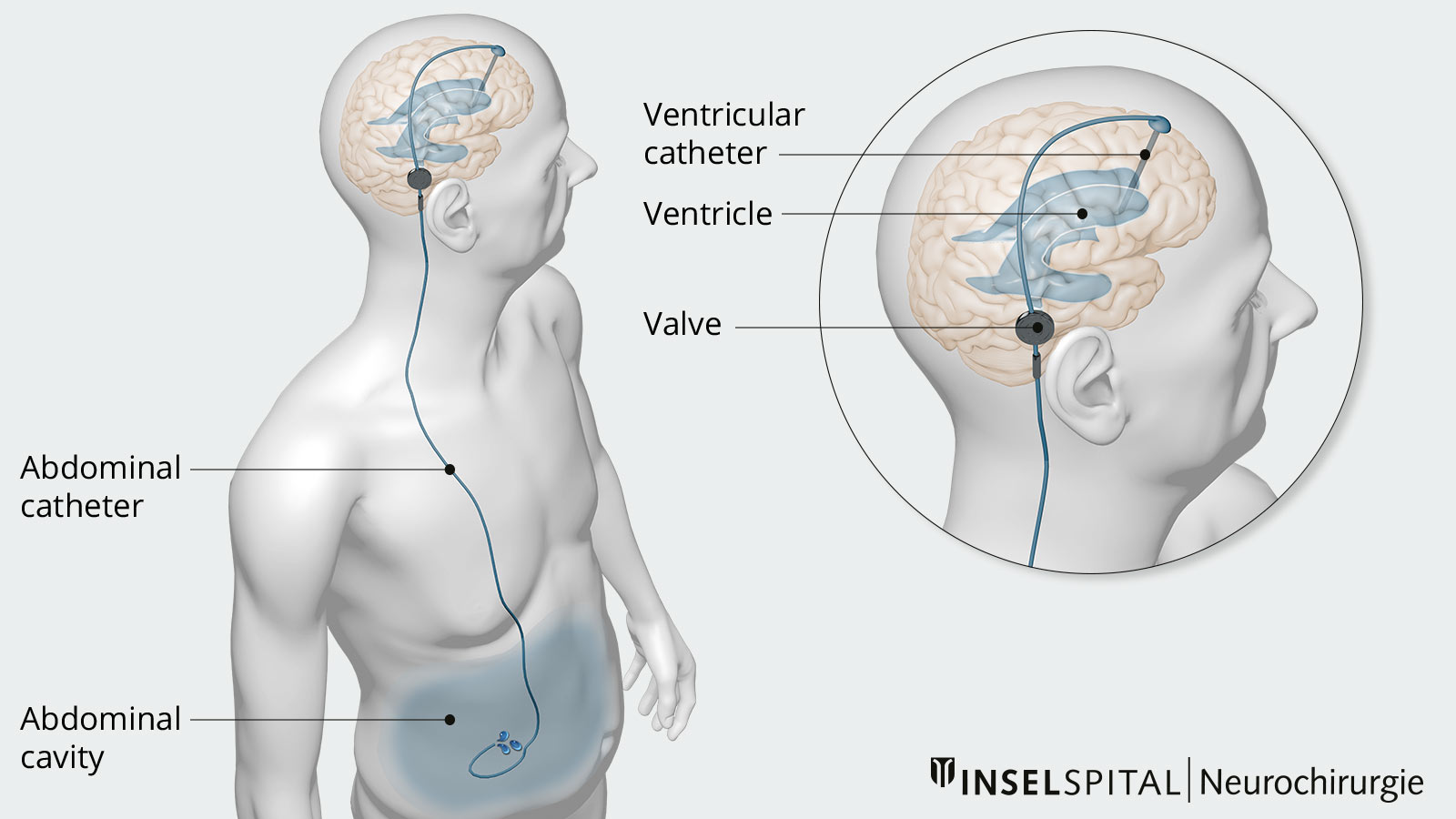
Ventriculoatrial shunt (VA shunt)
An alternative to drainage into the abdominal cavity is drainage directly into the atrium of the right side of the heart. This is a ventriculoatrial shunt or VA shunt for short. This variant may be necessary in the case of inflammation or severe adhesions in the abdominal cavity due to major previous operations.
Complications of shunt implantation
Shunt implantation is a simple and effective treatment for any type of hydrocephalus. The surgical complication rate is extremely low. However, even with an implanted shunt, complications and dysfunction may develop over time.
According to a prospective study from 2010, 9.7% of all shunt patients developed shunt dysfunction over time. For example, deposits of proteins from the cerebrospinal fluid can lead to malfunction or occlusion in the area of the valve or catheter. Moreover, catheters can deconnect or become infected over time. In such situations, a shunt revision with replacement of individual parts or the entire shunt system becomes necessary.
Why you should seek treatment at Inselspital
We have many years of expertise in the surgical treatment of hydrocephalus and are committed to the consistent advancement of our surgical expertise. For many forms of occlusive hydrocephalus, minimally invasive endoscopic creation of an alternative CSF outflow through a third ventriculocisternostomy is sufficient.
The latest technical equipment plays an important role in the success of the operation. Here at our Neurosurgery Department of Inselspital, we usually implant the position-dependent ProGav 2.0 valve from Miethke with an adjustable differential pressure unit and a gravitational unit during VP shunt surgery.
-
Schünke M, Schulte E, Schumacher U et al. PROMETHEUS Allgemeine Anatomie und Bewegungssystem. Thieme; 2018.
-
Webseite von Radiopaedia zum Thema Hydrocephalus (in englischer Sprache).
-
Urbán PP, Caplan LR (Eds.) Brainstem Disorders. Springer Nature; 2011.
-
Beez T, Sarikaya-Seiwert S, Steiger HJ, Hänggi D. Real-time ultrasound guidance for ventricular catheter placement in pediatric cerebrospinal fluid shunts. Childs Nerv Syst. 2015;31:235-241.
-
Sprung C, Schlosser HG, Lemcke J et al. The adjustable proGAV shunt: a prospective safety and reliability multicenter study. Neurosurgery. 2010;66:465-474.