If an infarct occurs in certain regions of the brain, it can cause chronic pain in affected patients. Physicians also refer to this pain as central neuropathic pain syndrome or central post stroke pain (CPSP). Conventional therapies and medications often have an inadequate response to this type of pain. In these cases, deep brain stimulation can provide pain relief. In the following, we provide an overview of the causes of this pain syndrome and the neurosurgical treatment options at Inselspital.
How does pain develop after a stroke?
Pain perception is an activity of the brain. Certain regions of the brain are involved in pain processing and integrate the sensory and also affective perceptual content into the overall experience of “pain”. What people perceive as painful is made up of several components:
- Pain localization
People can usually assign pain to one or more parts or regions of the body. - Pain quality
People experience different qualities of pain, such as a stabbing, pulling, sharp or burning pain. - Vegetative component
Pain is accompanied by a vegetative reaction such as changes in heartbeat, breathing or blood pressure. - Affective component
In addition, pain is associated with a highly unpleasant feeling, which is experienced as agonizing and suffering and is clearly differentiated emotionally from other unpleasant feelings such as sadness, fear or anger.
All these components are processed in different areas of the brain and combined to form the experience of pain. The structures involved in signal processing include the nerves, the spinal cord, the thalamus, various nucleus in the brainstem and hypothalamus, the amygdala und certain areas of the cerebral cortex. The structures involved in pain processing can be summarized as the pain network.
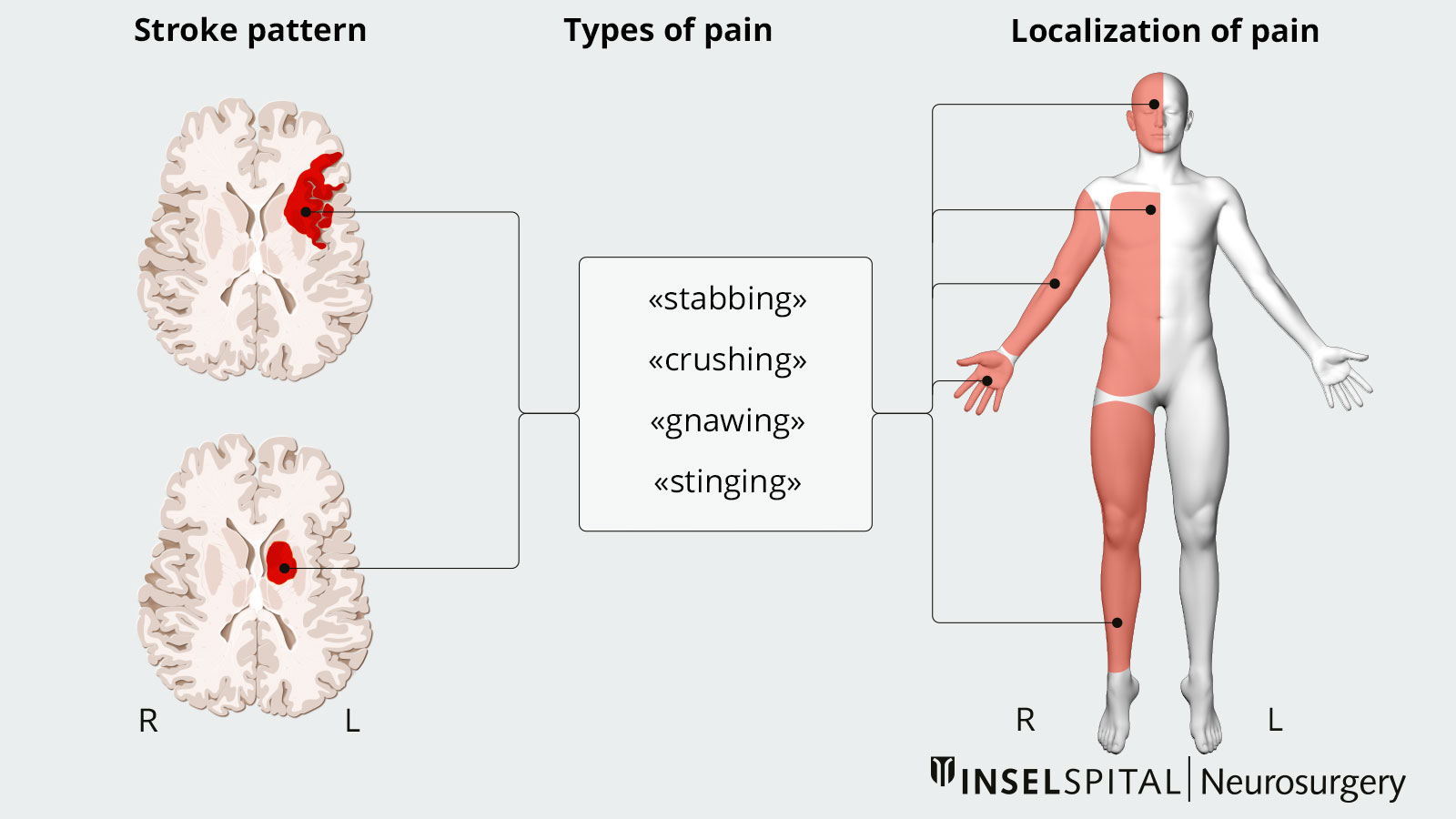
After a damage to one of these neuronal components of the pain network, as can be the case in a stroke, for example, chronic pain can occur, which is referred to as neuropathic pain. In the case of a lesion of the thalamus or the surrounding nerve tracts, this pain is also called central pain or thalamic pain *. The exact mechanisms at the cellular level are still largely unknown. It is estimated that up to 20% of patients develop a central pain syndrome after a stroke.
How does this central pain manifest itself?
A lot of patients describe the central neuropathic pain as burning pain. Shooting pain or throbbing pain are also typical. Usually, the opposite side of the body to the stroke is affected. In the case of an infarction of the left thalamus e.g., pain is felt in the right side of the body. Although the pain may occur immediately after the stroke, it usually starts a few weeks to months after the event.
What are the treatment options?
Drug therapy
Drug therapy is the first choice for treating neuropathic pain after a stroke. Typical analgesics such as paracetamol, ibuprofen, and novalgin are usually ineffective. Substances used include gabapentin, pregabalin or carbamazepine, as well as opiates or agents from the antidepressant group. Because of the potential side effects, drug treatment should be ordered and monitored by an experienced pain management specialist.
Transcutaneous nerve stimulation
Another therapeutic option is transcutaneous nerve stimulation (TENS). TENS is a current stimulation therapy used to stimulate muscles and treat pain.
Deep brain stimulation (DBS)
If the pain does not respond adequately to the classic therapies, deep brain stimulation (DBS) is an alternative treatment.
Clinical studies on DBS
In summary, studies on the efficacy of DBS for central pain remain conflicting. Chronic pain has been treated with deep brain stimulation since the 1950s *. This has involved stimulation of multiple target points in the human brain. All these target points have in common that they belong to the pain network in the brain.
Interestingly, in the 1970s, DBS was then considered a safe and effective therapy only for chronic pain syndromes – and not for movement disorders. Today, by contrast, it is precisely movement disorders that make up a large proportion of the indications for DBS.
The therapeutic efficacy for chronic pain was questioned after the publication of two larger, multicenter studies in 1976 and 1990. These studies failed to achieve the desired effect of a 50% improvement in pain in at least 50% of patients *. However, these studies were criticized by many experts. Ultimately, it must be concluded that these studies do not meet today's scientific standards and are therefore of little significance in our view.
Other studies since the 1990s published fluctuating success figures between 24–83% *.
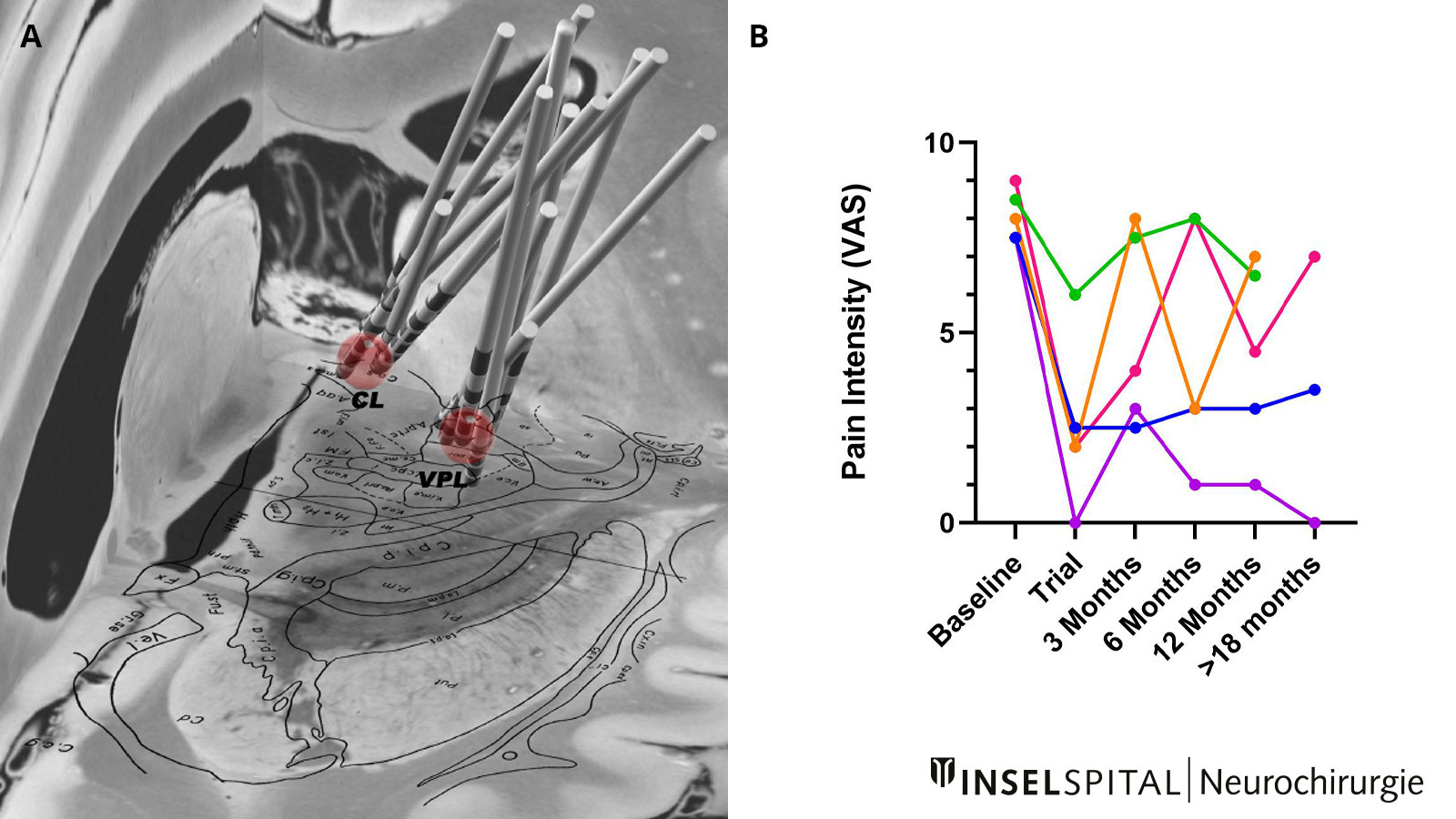
From our own experience, about half of patients with central pain after stroke benefit from DBS. The results between the respective patients vary between 0 and 100% of the perceived pain intensity *.
Most studies and also our experience show that in many patients, despite initially good efficacy on pain, there is a loss of effect over time and the stimulation settings have to be changed several times. Since only about 100 patients with chronic post-stroke pain have been treated with deep brain stimulation worldwide, 10 of them at the Inselspital in Bern, the actual efficacy of DBS for central post-stroke pain cannot be conclusively assessed at this time.
Current: Burst DBS study at Inselspital
Habituation effects to DBS are the crucial factor in long-term therapy failure. For this reason, we believe it is urgently necessary to explore alternative forms of stimulation in the hope of improving long-term outcomes in DBS therapy.
At Inselspital, to the best of our knowledge, the world's first prospective randomized study on the effectiveness of deep brain stimulation in the treatment of central pain syndromes is underway.
In our trial, we are comparing the efficacy and safety of two different forms of stimulation: normal deep brain stimulation with Burst deep brain stimulation. For this purpose, 20 patients with central pain after stroke or neuropathic facial pain (zoster neuralgia, neuropathic pain after injury, after dental treatment or maxillofacial surgery, etc.) are included in our trial.
If you are a patient and interested in enrolling in our Burst DBS study, please contact the principal investigator, PD Andreas Nowacki, MD.
Before the actual surgery, a very good patient selection is the prerequisite for the success of the treatment. Not all patients are suitable candidates for DBS surgery.
The indication must be discussed and jointly made by neurologists, neurosurgeons, neuropsychologists and psychiatrists on an interdisciplinary basis. All potential candidates are discussed at Inselspital within the context of an interdisciplinary board. Here, the indication, advantages and disadvantages of certain treatment alternatives to DBS (focused ultrasound), the exact target point with the expected effects and side effects are discussed in the context of the patient's respective clinical picture and his individual needs. Criteria such as operability and other concomitant factors (e.g., neuropsychological findings, concomitant psychiatric disorders) are also considered.
-
Treister AK, Hatch MN, Cramer SC, Chang EY. Demystifying Poststroke Pain: From Etiology to Treatment. PM R. 2017;9:63-75.
-
Pereira EA, Green AL, Aziz TZ. Deep brain stimulation for pain. Handb Clin Neurol. 2013;116:277-294.
-
Coffey RJ. Deep brain stimulation for chronic pain: results of two multicenter trials and a structured review. Pain Med. 2001;2:183-192.
-
Marchand S, Kupers RC, Bushnell MC, Duncan GH. Analgesic and placebo effects of thalamic stimulation. Pain. 2003;105:481-488.
-
Nowacki A, Zhang D, Barlatey S, Ai-Schläppi J, Rosner J, Arnold M, Pollo C. Deep Brain Stimulation of the Central Lateral and Ventral Posterior Thalamus for Central Poststroke Pain Syndrome: Preliminary Experience. Neuromodulation. 2022 Oct 17:S1094-7159(22)01268-5.
