Dorsal root ganglion (DRG) stimulation is a newer method for treating chronic pain. It is one of the therapeutic options grouped under the term neuromodulation. The dorsal root ganglion is a bundle of nerve cell bodies and nerve fibers that filters all sensory and painful stimuli. If the pain is very severe and all other therapeutic measures are ineffective, the respective nerve can be selectively stimulated using weak electrical currents. This blocks the transmission of pain through the dorsal root ganglion.
When is dorsal root ganglion stimulation used?
DRG stimulation is used for the following conditions:
- complex regional pain syndrome (causalgia, Sudeck's disease)
- thoracic neuropathies (after mastectomy, thoracotomy, herpes zoster)
- abdominal and visceral pain (chronic pancreatitis)
- inguinal and testicular pain (after inguinal hernia surgery)
- postoperative pain (e.g. shoulder, hand, hip, knee, foot, etc.)
- phantom and residual limb pain (after amputation)
- distal-occurring neuropathies (polyneuropathy, diabetes)
Patient selection is based on the same principle as for spinal cord stimulation. Patients with limited quality of life and high levels of suffering who have been treated conservatively, surgically or with medication are eligible for DRG stimulation. They are first evaluated by an interdisciplinary team of pain therapists, psychiatrists and neurosurgeons to determine whether they are suitable candidates for DRG stimulation.
How does dorsal root ganglion stimulation work?
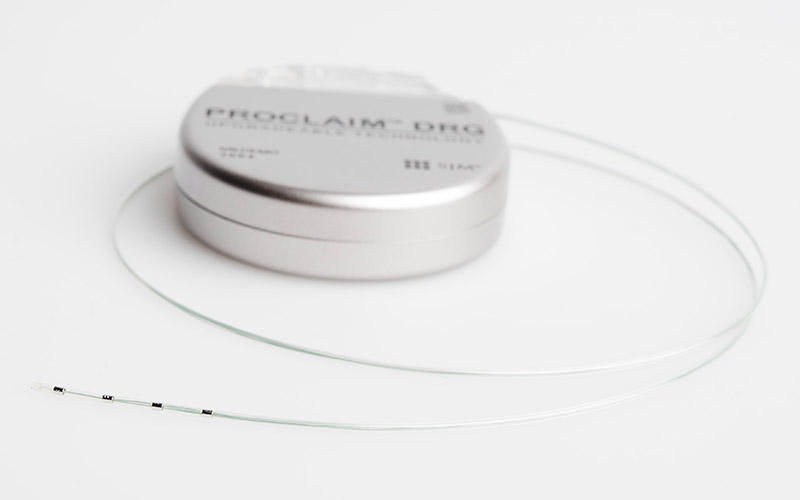
In principle, DRG stimulation works similarly to spinal cord stimulation with the difference that the electrode is not placed on the spinal cord but on the dorsal root ganglion. The dorsal root ganglion is a structure between the spinal cord and peripheral nerve that contains the cell bodies of sensitive nerve cells and is involved in the process of chronic pain generation and transmission. It represents an important interface for communication between peripheral and central nervous systems. The electrodes are implanted in a minimally invasive procedure under X-ray control. The level at which the electrode is implanted depends on the location of the pain.
What is the goal of dorsal root ganglion stimulation?
The primary goal is to improve quality of life. This includes:
- pain reduction by 50%.
- reduction in pain medication
- improvement in sleep quality
- increase in physical activity
- reintegration into the work process
- general improvement in psychological well-being
Although freedom from pain can be achieved in rare cases, this is not a realistic goal. Nor is it expected from this therapy.
What are the advantages and disadvantages of dorsal root ganglion stimulation?
Advantages
- Individual parts of the body, such as only the knee or only the foot, can be stimulated in a targeted manner, unlike the more extensive spinal cord stimulation.
- The complication rate of electrode displacement is lower.
- In addition, there are fewer unpleasant position-dependent body sensations (paresthesias) such as tingling,«formication» or numbness.
Disadvantages
- A disadvantage of DRG stimulation is the more demanding implantation technique.
Before surgery
Prior to surgery, a magnetic resonance imaging (MRI) scan must be performed to rule out possible obstructions to passage or narrowing of the neuroforamen.
In addition, a visit to our anesthesia consultation is necessary.
We will apply to the health insurance company to have the costs covered.
Those who are considered for dorsal root ganglion stimulation first undergo a test phase before the neurostimulator is definitely implanted. Before the test phase, a so-called paresthesia mapping – an assessment of the unpleasant body sensations – is carried out by the pain therapy colleagues. In this process, under X-ray and/or ultrasound guidance, current is administered externally to the dorsal root ganglion via a needle in order to better delineate the pain area in the form of tingling. This examination helps the neurosurgeons to determine the correct height of the electrode position as well as the number of electrodes required.
On the day of surgery
The patient arrives for the operation in the morning on an empty stomach. This is performed under spinal anesthesia. In the operating room, the electrodes are placed on the dorsal root ganglion under X-ray control. During the operation, the patient gives feedback whether the painful area is well covered by the paresthesias. If this is the case, the electrodes are connected under the skin to an extension that is led out of the skin in the trunk area. An external test stimulator is connected to this extension. The patient remains in the hospital for one night for monitoring and can be discharged home the next day.
The test phase lasts one to two weeks. Showering and bathing are not allowed during this time. Spitex is organized for regular dressing changes and wound control.
If the patient benefits from the stimulation, the definitive implantation of the neurostimulator, also known as a battery, is performed on an outpatient basis. This means that the patient arrives for the procedure in the morning and can go home the same evening. Before the patient goes home, an X-ray is taken to check the position of the electrodes.
If the patient does not respond to the therapy, the electrodes are removed.
Aftercare
The patient comes to our clinic after two weeks for suture removal and wound control. The stimulator is checked and the stimulation is adjusted. Further regular check-ups take place after 6 weeks, 3, 6 and 12 months, then at annual intervals. When the battery is empty, it must be replaced by a small operation under local anesthesia.
What are the complications?
The complication rate is low. However, as with any procedure, complications can occur.

