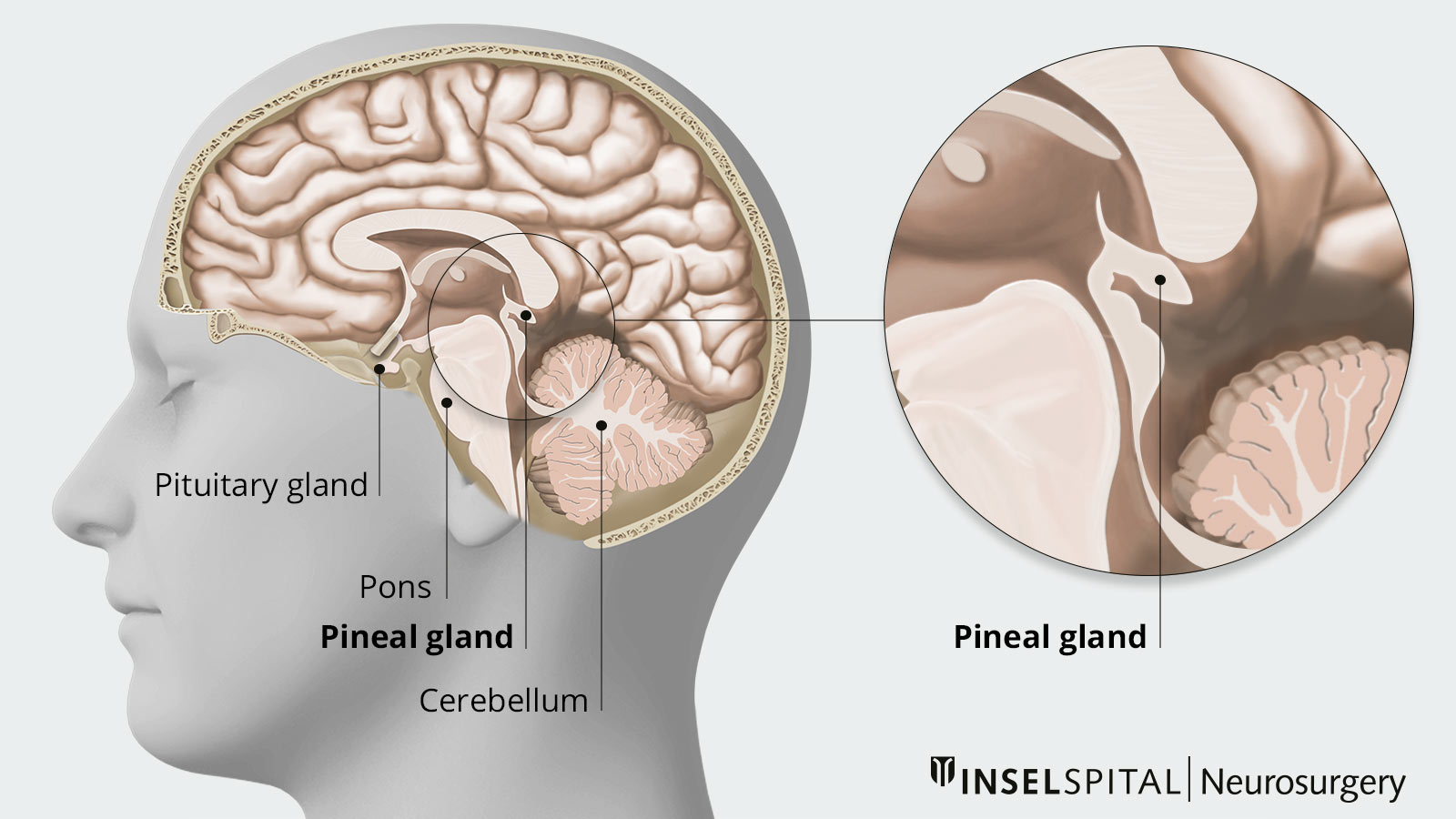
The tumors of the pineal region are called pineal tumors, tumors of the pineal gland or pinealomas. They are rather rare tumors. The pineal gland is a small endocrine gland located at the back of the midbrain. It is adjacent to the 3rd ventricle, a part of the cerebrospinal fluid drainage system. The pineal gland produces the hormone melatonin and is thus mainly responsible for controlling the sleep-wake rhythm of the human body.
Who is most commonly affected by a pineal tumor?
Pineal tumors account for 3–8% of brain tumors in children aged 1–12 years. In adults, they account for less than 1% of brain tumors, with males more commonly affected than females.
There are more than 17 different tumor types in the pineal region.
Germinomas are most commonly found (50–75%), followed by astrocytomas, teratomas, and pinealoblastomas. Some tumor types, such as germinal cell tumors, ependymomas, and pineal cell tumors, often spread via the cerebrospinal fluid outflow and lead to drip metastases *, *, *, *.
What are the symptoms of a pineal tumor?
Due to the anatomical location of the pineal gland, space-occupying lesions in this area typically result in pressure on the surrounding brain tissue (mass effect), causing the following symptoms:
- The leading symptom is a buildup of cerebrospinal fluid, also called hydrocephalus. Patients then usually suffer from headaches, nausea, fatigue or memory problems.
- On rare occasions, acute headache may also occur due to sudden hemorrhage or circulatory disturbance caused by the tumor.
- If brainstem compression occurs, patients may notice double vision or other eye movement problems.
- Sometimes hormonal disturbances may also occur if the tumor exerts pressure on the pituitary gland (hypophysis).
- In the case of drop metastases in the spine, these can constrict the spinal cord or nerve roots and lead to neurological deficits and pain *, *, *.
Imaging
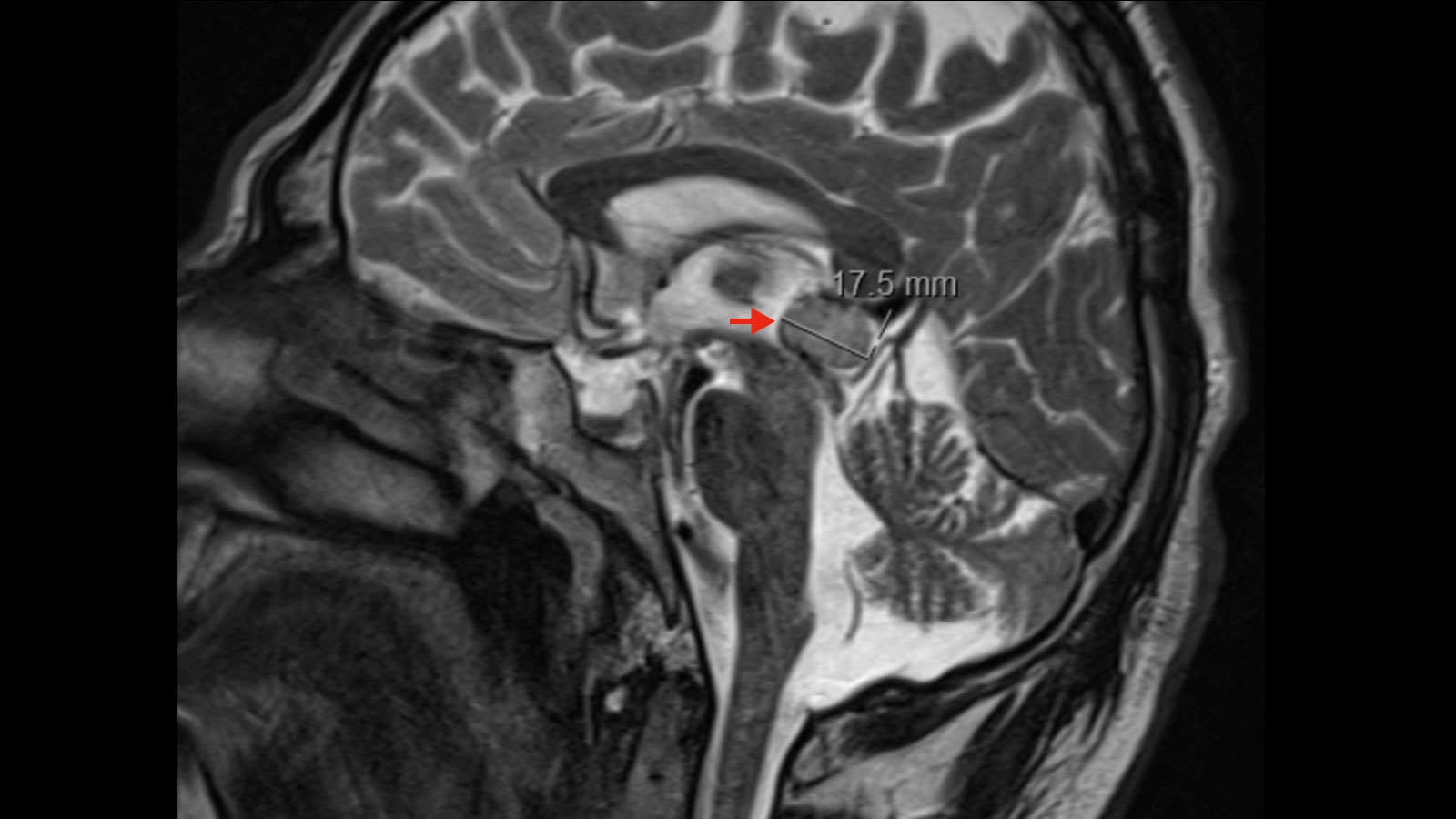
Magnetic resonance imaging (MRI) is considered the gold standard, showing abnormalities in the pineal area.
Occasionally, the cyst wall of a pinealis cyst can be visualized with the use of contrast material. Pinealis cysts are very common benign changes in the area of the pineal gland. However, irregularities of the cyst wall such as nodular changes may indicate a potentially malignant mass.
Insufficient for diagnosis is computed tomography (CT), in which the signal of the cyst often corresponds to that of the cerebrospinal fluid and can therefore also provide a false diagnosis.
In addition, it is recommended to complete the imaging diagnosis with supplementary MRI images of the entire spine to exclude drop metastases *, *.
Tumor marker
Some pinealis tumors, such as the germ cell tumors, may produce elevated tumor markers (beta-hCG, alpha-fetoprotein, placental alkaline phosphatase) in the CSF and blood. In cases with positive tumor markers, regular laboratory chemistry follow-up can be performed to assess treatment success or diagnose recurrence. However, tumor markers are not sufficient for diagnosis, since many tumors of the pineal region consist of mixed cells and do not necessarily have to show elevated tumor markers *, *, *.
Histology
For a definitive diagnosis, the tumor tissue must be analyzed on a histological basis. First, tissue from the tumor is surgically removed by resection or biopsy. The tissue is then processed by a pathologist. For this purpose, it is stained with special stains and analyzed and evaluated under the microscope *, *, *, *. It takes an average of 3–5 days to receive the fine tissue examination results.
What is the treatment for pineal tumors?
There are a variety of different types of pineal tumors that require different therapy. Here at Inselspital, the specific therapy is determined by our interdisciplinary tumor board consisting of neurosurgeons, neurologists, neuroradiologists, oncologists and radiation oncologists – depending on the results from the fine tissue examination and the tumor markers.
Pineal cell tumors
On the one hand, there is pineocytoma, a well-differentiated, benign tumor. In the case of pineocytoma, surgical resection is the treatment of choice. If complete resection is not possible, surgery is followed by complementary radiotherapy.
On the other hand, there is pineoblastoma, a malignant tumor that belongs to the primitive neuroectodermal tumors (PNET).
Both pineocytoma and pineoblastoma can metastasize via CSF drainage and respond well to radiotherapy. However, radiotherapy is not recommended for children under 3 years of age. This is because of the increased side effects on the still-developing brain.
Without treatment, 91% of patients show tumor growth within 2 years. In contrast, over 50% of treated patients continue to show stable conditions after 5 years *, *, *.
Germ cell tumors
Germ cell tumors are divided into germinomas and non-germinomatous germ cell tumors (NGGCT).
Germinomas usually do not require resection and can be treated with radiotherapy only. In this case, a 10-year survival rate of > 90% is shown.
In NGGCT, a further distinction is made between embryonal carcinomas, choriocarcinomas and endodermal sinus tumors (yolk sac tumors). These are treated by radiochemotherapy, a combination of radiotherapy and chemotherapy *, *, *.
Pineal cysts
Pineal cysts are benign masses that usually do not cause any symptoms as long as they are not larger than 1–2 cm. A pineal cyst is found as an incidental finding in about 4% of all head MRIs performed. In children, regular imaging checks are performed because of the potential for cyst growth. In adults, cysts are usually stable, so follow-up MRI is recommended only if symptoms are present. If the cysts grow or cause symptoms, surgical resection is recommended. The success rate of surgery is 90–95% *, *, *.
Procedure of the surgery
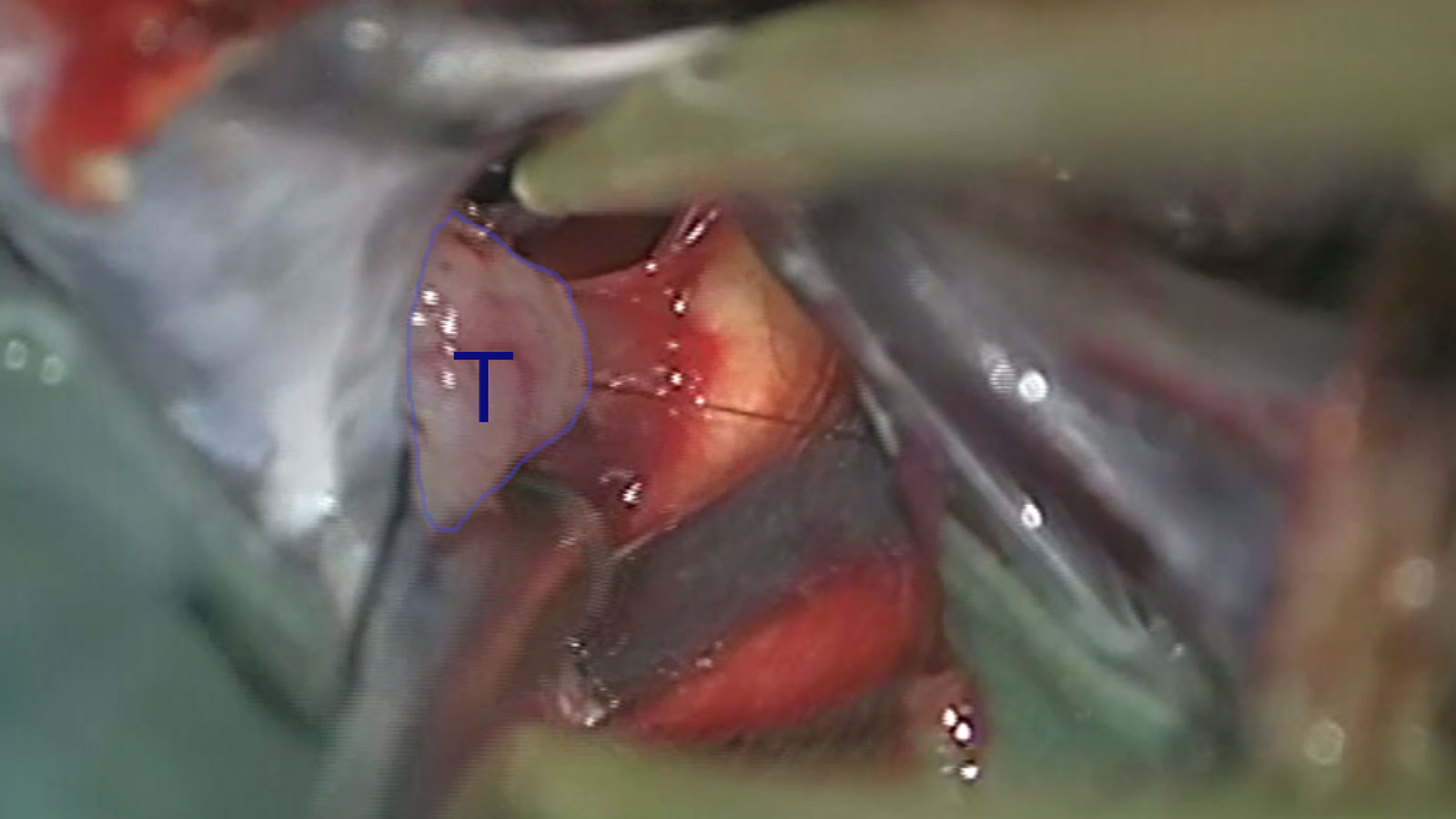
For the surgery, the patient's head is fixed with a 3-point holder. With the help of neuronavigation, the most recent MRI images of the patient are matched with the current fixed head position.
After the skin incision, the skull bone is opened with a special bone saw. This is most usually performed from behind, above the cerebellum in the border between the cerebrum and the cerebellum (infratentorial supracerebellar approach). Usually, it can be approached from the midline, but the exact access route is planned and determined by the surgeon based on MRI images and the exact location of the tumor.
The meninges, also called dura, follow below the skull bone and are opened in the next step.
Under microscopic control and with the aid of neuronavigation, the tumor is exposed with as little tissue damage as possible, taking into account the surrounding structures. Once this is done, the resection is performed. The maximum extent of resection depends on the extent to which the tumor has infiltrated the surrounding tissue.
After thorough hemostasis, the dura is tightly closed again.
The previously removed skull bone is correctly repositioned and fixed in place using thin titanium plates and screws.
Finally, the wound is closed with staples or sutures.
After surgery, patients come to our monitoring ward for close neurological monitoring. With a normal course, patients can usually be transferred back to the ward on the 1st or 2nd day after surgery. During this period, a new MRI is also performed to check the extent of resection postoperatively. Further therapy planning depends on this *, *, *.
Treatment alternatives
In patients with hydrocephalus, internal CSF drainage via a ventriculoperitoneal shunt may be considered as an alternative. An endoscopic third ventriculocisternostomy (ETV), in which a short-circuit connection is made between the internal and external cerebrospinal fluid spaces, may also be considered. Here, however, samples of the cyst are not taken for examination *, *, *, *.
-
Greenberg MS. Handbook of Neurosurgery. Thieme; 2016:1664.
-
Harbaugh R, Shaffrey CI, Couldwell WT. Neurosurgery Knowledge Update. Thieme; 2015:984.
-
Zaazoue MA, Goumnerova LC. Pineal region tumors: a simplified management scheme. [editorial]. Childs Nerv Syst 2016;32(11):2041.
-
Sonabend AM, Bowden S, Bruce JN. Microsurgical resection of pineal region tumors. J Neurooncol. 2016;130:351-366.
-
Májovský M, Netuka D, Beneš V. Clinical management of pineal cysts: a worldwide online survey. Acta Neurochir (Wien). 2016;158:663-669.