It is estimated that up to 1 million people in Switzerland suffer from migraines. Like cluster headaches, migraines are classified as seizure-like headaches. In most cases, a migraine can be successfully treated with medication. When migraine pain is chronic and medication does not work, there are functional neurosurgical treatment options such as occipital nerve stimulation.
What is a migraine?
A migraine is usually characterized by a pulsating, seizure-like headache, usually on one side of the head. The headaches are often accompanied by vegetative symptoms such as nausea, vomiting and sensitivity to light. A typical migraine attack usually lasts between several hours and 3 days.
In some cases, migraines can also occur chronically. In this case, patients suffer from migraine headaches more than 15 days a month for at least three consecutive months. An estimated 2% of the population is affected by chronic migraine *.
What are the treatment options?
Drug therapy
Drug therapy is always the first choice in treating migraine. Here, we distinguish between drugs for acute attack treatment (non-steroidal anti-inflammatory drugs such as ibuprofen or triptans) and drugs for relapse prophylaxis (metoprolol, flunarizine, topiramate, etc.). Because of the potential side effects, drug treatment should be administered and monitored by an experienced neurologist.
Neuromodulation – occipital nerve stimulation
If a migraine becomes chronic and does not respond adequately to drug therapies, a neuromodulatory procedure may be considered. Occipital nerve stimulation (ONS) is a possible treatment alternative in this case.
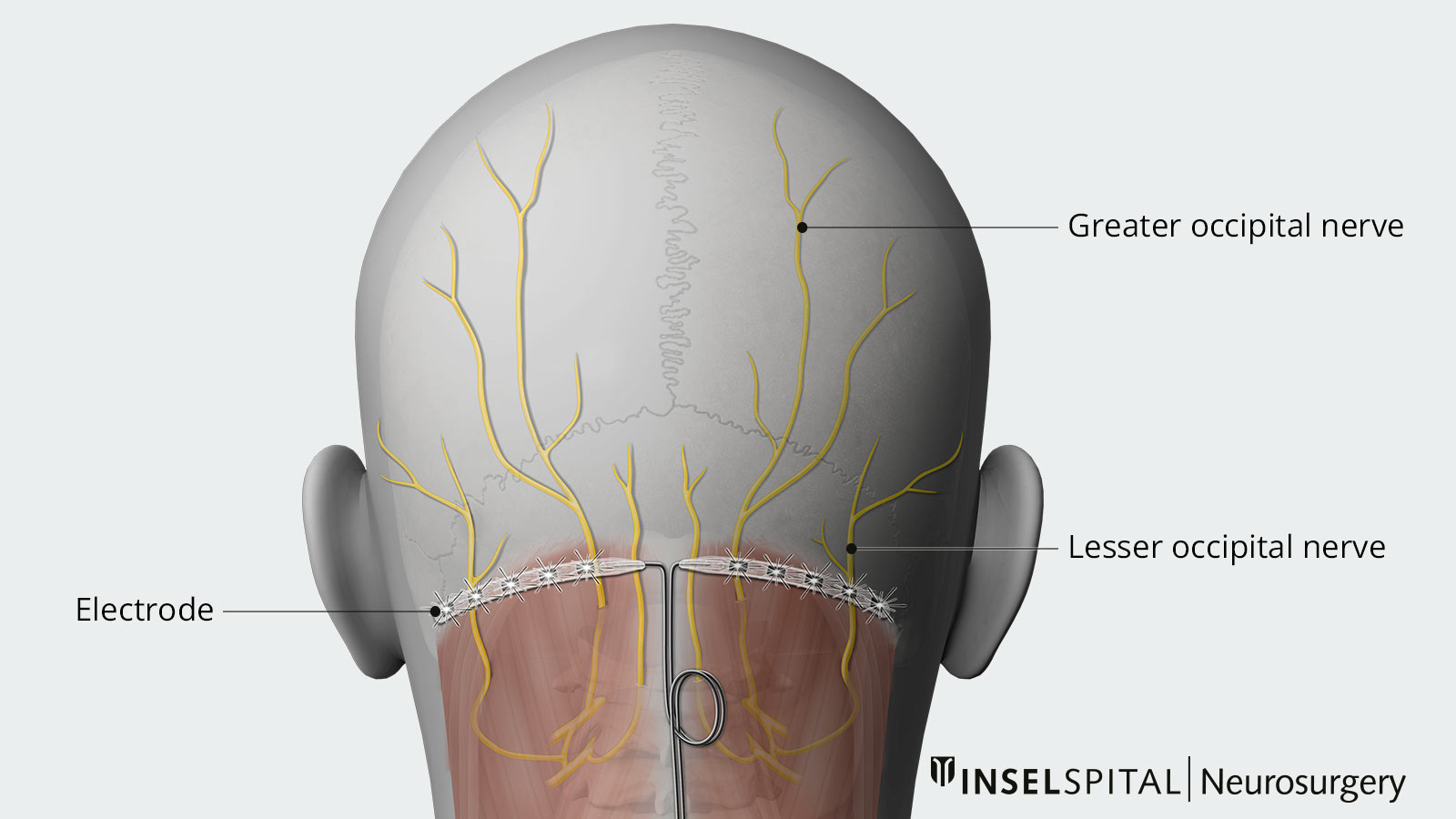
During ONS, electrodes are inserted under the skin in the suboccipital fatty tissue in the occipital region (see illustration). The aim is to stimulate the large and small occipital nerves. The electrodes are connected to a pacemaker, which is usually implanted below the collarbone.
Studies on occipital nerve stimulation (ONS)
So far, only a few high-quality studies have been published to test the efficacy of ONS in chronic migraine. Overall, the randomized controlled trials and prospective cohort studies to date show a moderate effect of ONS in the treatment of chronic migraine.
The largest multicenter randomized controlled trial to date was conducted by Silberstein et al. in the United States in 2012. After a successful test phase, patients were divided into two groups, group A with active stimulation and group B with stimulation switched off. The patients were required to maintain a pain diary. After 12 weeks, the results of the two groups were compared. There was no significant difference between the groups when response rate was strictly defined (at least 50% pain reduction): in group A (active stimulation), 17% of patients met this requirement compared to 13.5% in group B (inactive stimulation). However, overall stimulation demonstrated a significant difference in pain reduction of at least 30%: 40% in group A (active stimulation) versus 16% in group B (inactive stimulation). Furthermore, patients experienced a significant reduction in the number of pain attacks per month *.
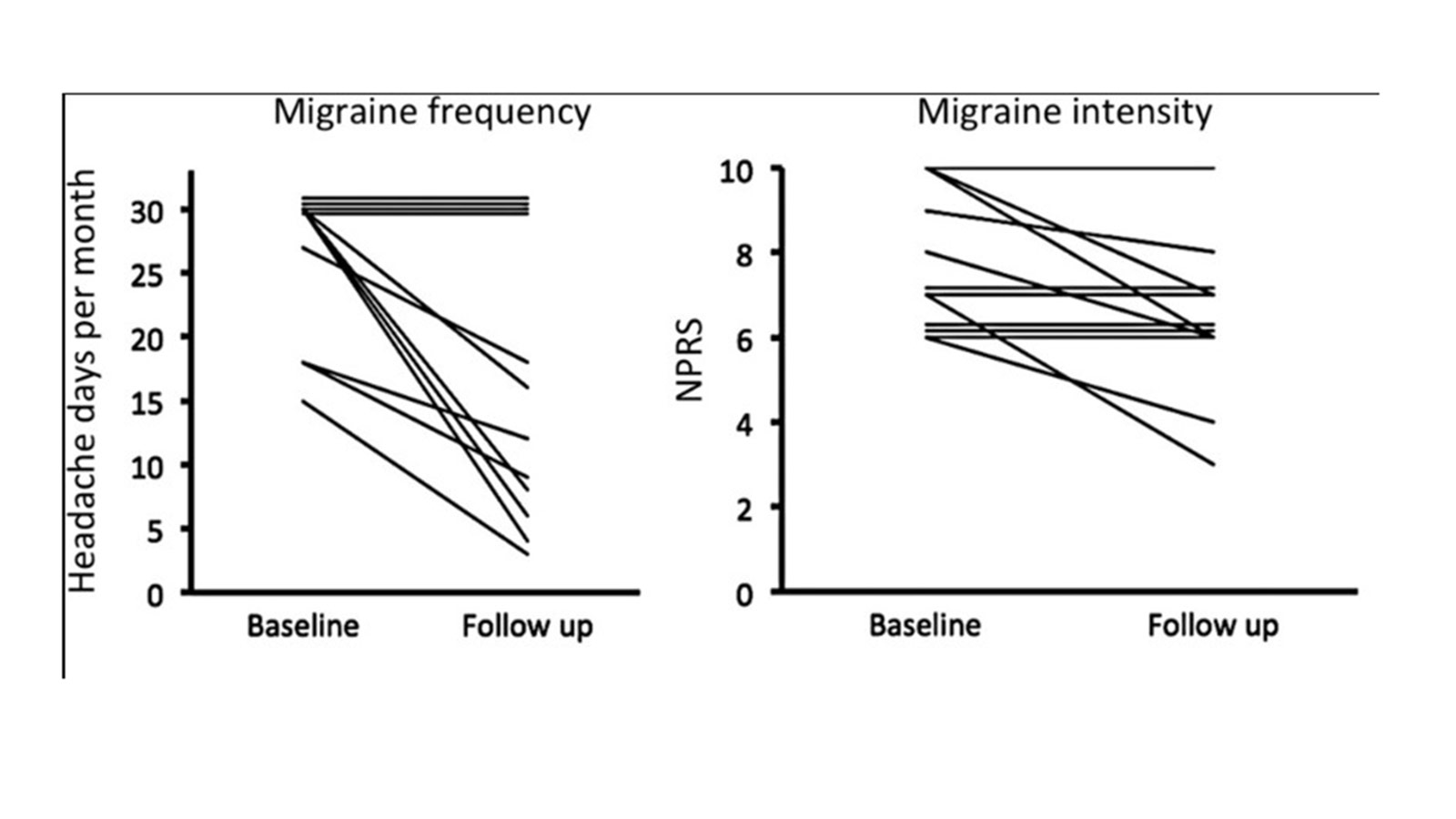
In addition, several prospective cohort studies demonstrated the long-term effect of therapy *.
It is worth mentioning a recent paper by the Functional Surgery Group from Oxford, which presents the results of a new form of stimulation in connection with occipital nerve stimulation. The colleagues carried out burst stimulation of the occipital nerve. All in all, the results for the treatment of chronic migraine are mixed. Interestingly, however, there is a subgroup of patients who do not respond to ONS at all, as well as a subgroup of patients with a very good response and a reduction in attack frequency of up to 90 %. *
-
Saper JR, Dodick DW, Silberstein SD et al. Occipital nerve stimulation for the treatment of intractable chronic migraine headache: ONSTIM feasibility study. Cephalalgia. 2011;31:271-285.
-
Silberstein SD, Dodick DW, Saper J et al. Safety and efficacy of peripheral nerve stimulation of the occipital nerves for the management of chronic migraine: results from a randomized, multicenter, double-blinded, controlled study. Cephalalgia. 2012;32:1165-1179.
-
Miller S, Watkins L, Matharu M. Long-term outcomes of occipital nerve stimulation for chronic migraine: a cohort of 53 patients. J Headache Pain. 2016;17:68.
-
Garcia-Ortega R, Edwards T, Moir L, Aziz TZ, Green AL, FitzGerald JJ. Burst Occipital Nerve Stimulation for Chronic Migraine and Chronic Cluster Headache. Neuromodulation. 2019 Jul;22(5):638-644.
